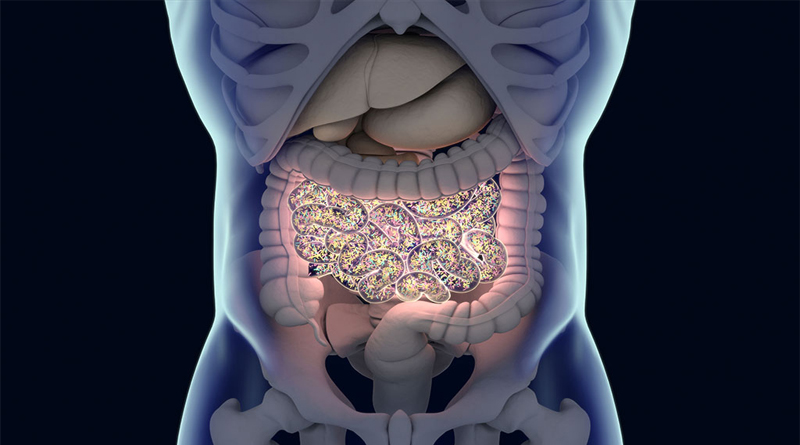
The way in which the gut microbiome contributes to human health has been the subject of considerable research, with the quality of the microbial community linked to our ability to stay healthy, fight off pathogens, and improve immune responses. Now researchers at the Stanford University School of Medicine have demonstrated that it’s possible to promote the growth of a specific bacterial community in mice by controlling the diet of the mice—findings that may ultimately lead to new disease-fighting therapies, the researchers report. Results of the research were published this spring in the journal Nature.
“Although we continue to acquire new strains [of bacteria in the gut] throughout life, this acquisition is a poorly orchestrated and not well understood process,” says Stanford researcher Justin Sonnenburg, associate professor of microbiology and immunology. “This study suggests it could be possible to reshape our microbiome in a deliberate manner to enhance health and fight disease.”
The research that Sonnenburg and his team conducted involved collecting effluent from a wastewater treatment facility to find members of the Bacteroides family with the ability to digest a marine polysaccharide called porphyran that is contained in nori, a kind of seaweed, and is uncommon in American diets. The gene cluster that makes it possible for a bacterium to digest porphyran rarely occurs in people who don’t consume seaweed regularly.
After identifying this particular bacterial strain (i.e., one capable of digesting porphyran), the researchers experimented with introducing it into three groups of laboratory mice—two groups that had their own gut bacteria eliminated and replaced with bacteria from humans and one group that did not. Among mice fed a typical mouse chow diet, the porphyran-digesting strain either didn’t engraft in the any of the mice’s microbiomes or did so only to a limited extent. However, when test groups of mice were fed diets rich in porphyran, the bacteria engrafted at similar levels in mice in all of the groups. And the extent to which it engrafted was directly affected by the amount of nori the mice consumed. “The direct effect of diet on the bacterial population was very clear,” says Sonnenburg.
Lead study author and former Stanford graduate student Elizabeth Shepherd says the researchers chose to work with the Bacteroides bacteria because it is the most abundant genus in the healthy American gut and genetic tools for engineering these bacteria with the potential to express therapeutic genes have been developed. Thus, these bacteria provide a safe vehicle for introducing therapeutic genes into the gut, and because of their greater abundance, they are likely to have a greater therapeutic impact than a strain that only colonizes the gut at low levels.
The research was revelatory in multiple ways. “While one significant outcome is our ability to control colonization of strains of interest into divergent microbiomes, the research highlights the importance of diet in shaping the community of microbes in the gut,” says Shepherd. “As we learn more about how to feed our microbes, we consistently find that eating foods rich in diverse microbiota accessible carbohydrates (the main components of dietary fiber) promotes bacterial diversity and production of beneficial compounds from gut microbes.”
Sonnenburg sees a future in which the ability to manipulate human gut microbial communities will lead to exciting new options in medical treatment. For example, he says, “A physician whose patient is about to begin immunotherapy for cancer may choose to also administer a bacterial strain known to activate the immune system. … Conversely, a patient with an autoimmune disease may benefit from a different set of microbiota that can dial down an overactive immune response. They are just a very powerful lever to modulate our biology in health and disease.”
Shepherd is cofounder of a San Francisco–based start-up called Novome Biotechnologies that is working to engineer bacteria from the human gut microbiome to treat disease.
Source: IFT